Metabolic Research Institute Inc.
PERFORMING CLINICAL TRIALS IN WEST PALM BEACH SINCE 1996
MRI is now offering liver scans via FIBROSCAN technology at no cost!
A FIBROSCAN is a simple, painless and non-invasive procedure used to accurately assess the health of the liver. Individuals determined to have liver damage may be eligible to participate in clinical studies that may help.



About Metabolic Research Institute Inc.
Metabolic Research Institute’s clinical trials are the fastest and safest ways to find treatments that work and improve people’s health. Whether it’s diabetes, high blood pressure, heart disease, high cholesterol, or a variety of other health issues, clinical research studies provide the medicine of tomorrow… today.
Metabolic Research Institute, Inc. (“MRI”), is a private Clinical Research Company located at 1515 North Flagler Drive, Suite 440, West Palm Beach Florida 33401. Unless otherwise noted, all study-related appointments for qualified clinical participants in any MRI research trial will take place at this address.
FROM OUR BLOG

Nonsegmental Vitiligo Study
New Vitiligo Study - Now Enrolling West Palm Beach, Florida New research study enrolling in West Palm Beach, FL for people who have nonsegmental vitiligo (white patches of skin) on the face and body. Researchers are testing an investigational oral medication. •...
Concerned about fatty liver?
Fatty Liver Disease (NASH) Clinical Research Study Enrolling Now in West Palm Beach FL The SYNCHRONY Histology study is a clinical study to see what effect an investigational drug, EFX, has on scarring of the liver in NASH. AII participants will need to have NASH...
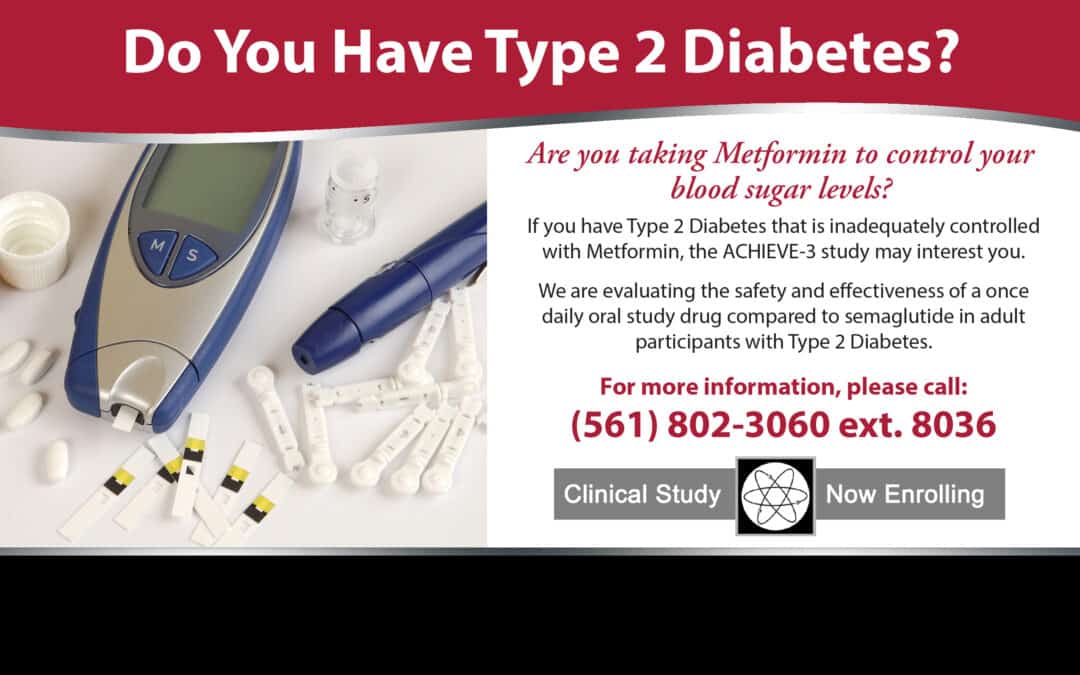
DM2 on Metformin
Clinical study enrolling now in West Palm Beach, FL ACHIEVE - 3 ACHIEVE-3 is a clinical research study for people with Type 2 Diabetes who are being treated with metformin. The study will test if an investigational medicine (the medicine being studied) can help with...